While most allergic responses are mild, anaphylaxis represents a critical escalation. It is a rapid-onset, potentially fatal condition triggered by allergens such as food, medication, insect venom, or latex. Immediate recognition and intervention are non-negotiable. Effective first aid response can halt the progression to systemic shock and prevent biphasic recurrence within 12 hours of the initial reaction.
Progression from Mild Symptoms to Crisis
Anaphylaxis may begin with seemingly benign symptoms such as skin rash or nasal discharge. However, this can swiftly evolve into multi-system failure without warning.
Escalation Signs Include:
- Breathing difficulty
- Swelling of face, lips, or tongue
- Tightening of the throat
- Dizziness or loss of consciousness
- Abdominal pain, vomiting, diarrhoea
- Weak pulse or cardiac arrest
Even a history of mild reactions is not predictive of future severity. All individuals with known allergies require an action plan and access to adrenaline at all times.
Establishing Clinical Diagnosis
Formal evaluation by a qualified allergist is essential. Diagnosis includes patient history and confirmatory tests such as:
- Skin prick testing
- Oral food challenges
- Blood-specific IgE assays
Referral Indicators:
- Recurring or escalating allergic symptoms
- Unidentified triggers
- Possible eligibility for immunotherapy
- Co-morbid conditions complicating allergy control
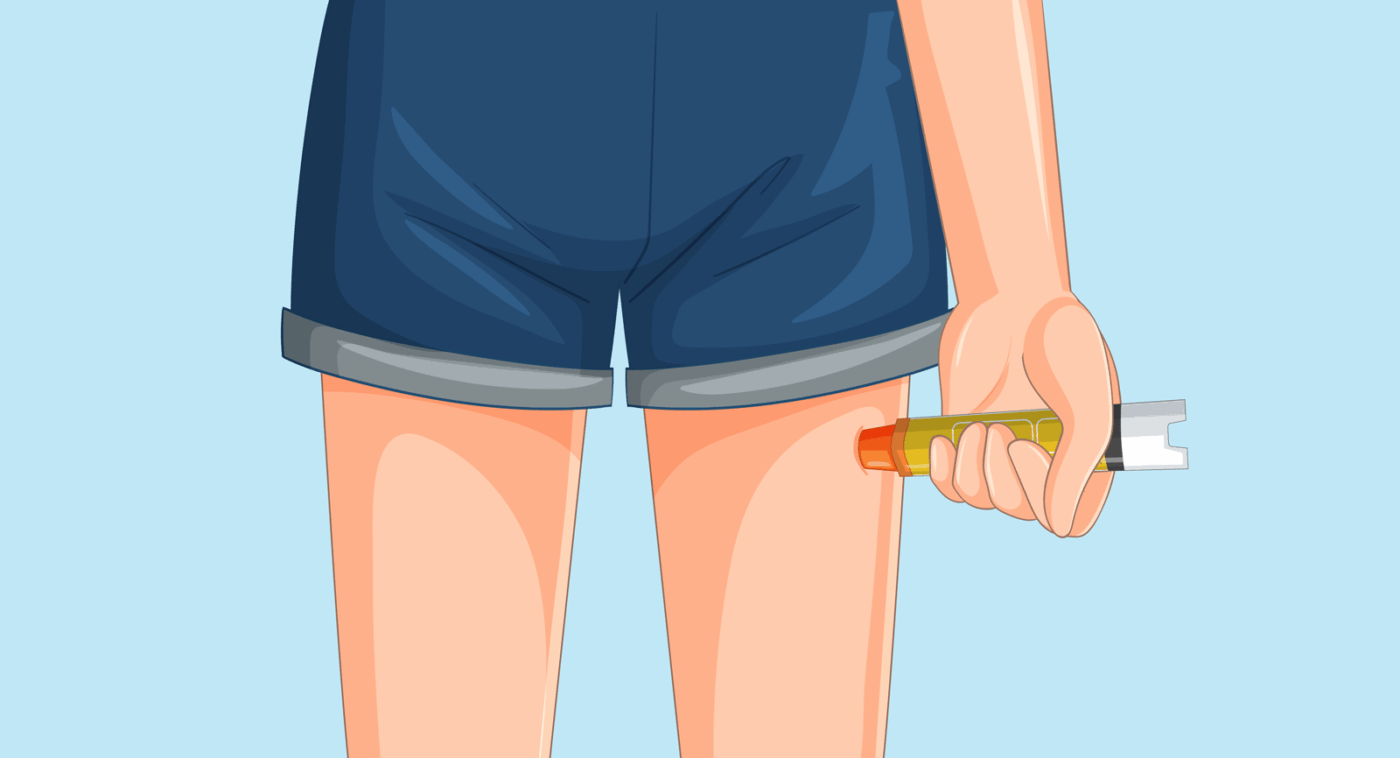
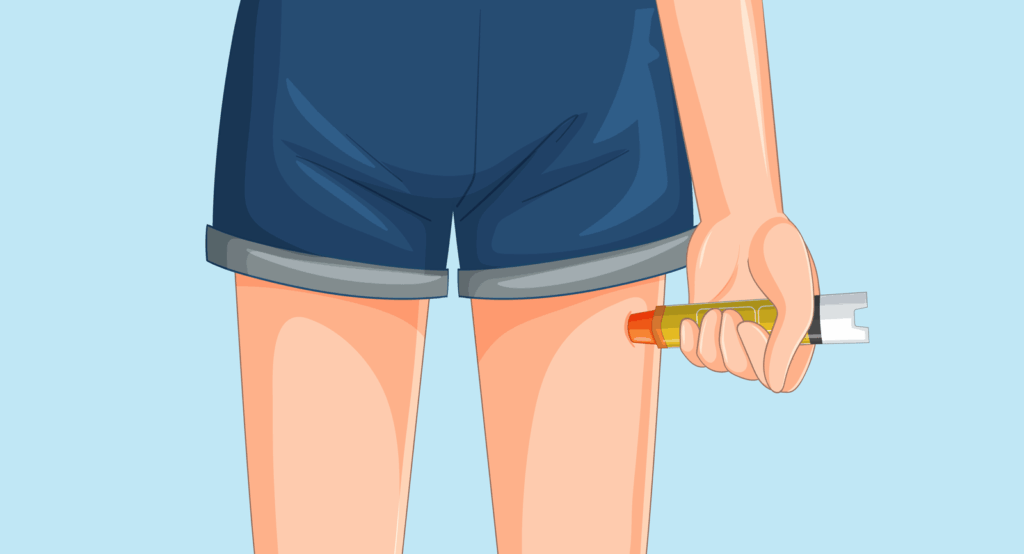
Emergency Management Protocols
First-line treatment for anaphylaxis is intramuscular administration of epinephrine. Secondary doses may be necessary. Auto-injectors must be accessible at all times. Adrenaline should be administered at the first sign of systemic involvement, not delayed.
Risk Minimisation Tactics:
Trigger avoidance is the highest form of prevention. Consult with an allergist for tailored strategies. Categories of common anaphylaxis triggers include:
- Foods: peanuts, tree nuts, dairy, eggs, shellfish
- Latex: present in gloves, adhesives, tubing
- Medications: antibiotics, NSAIDs, anaesthesia
- Insect stings: bees, wasps, ants
Contextual Avoidance Techniques:
- Medication: Disclose known reactions to all healthcare providers. Request desensitisation protocols when avoidance is not possible.
- Food: Inspect all labels. At restaurants, confirm preparation methods. Inform school staff and maintain emergency medication for children.
- Insects: Wear neutral clothing. Avoid fragrances. Do not walk barefoot. Cover drink containers.

Image source: Australia Wide First Aid
Post-Crisis Procedure
Following an anaphylactic episode, call 111—even after epinephrine administration. Identification of the trigger aids in future risk mitigation. Post-incident review by an allergist is mandatory.
For structured training in emergency identification, medication administration, and risk management, enrol in our online Anaphylaxis First Aid course. For institutional and workplace risk strategy, the Workplace Anaphylaxis Risk Management course covers compliance protocols and emergency planning. If your environment includes overlapping risks, Workplace Asthma and Anaphylaxis Management provides integrated response training.
All courses are fully online and include certification. Ensure you’re prepared to intervene effectively during anaphylactic emergencies, in both personal and professional contexts.